Understanding Pre-Exposure Prophylaxis: A Guide to PrEP Medicine
Why PrEP Matters: Orientation and Outline
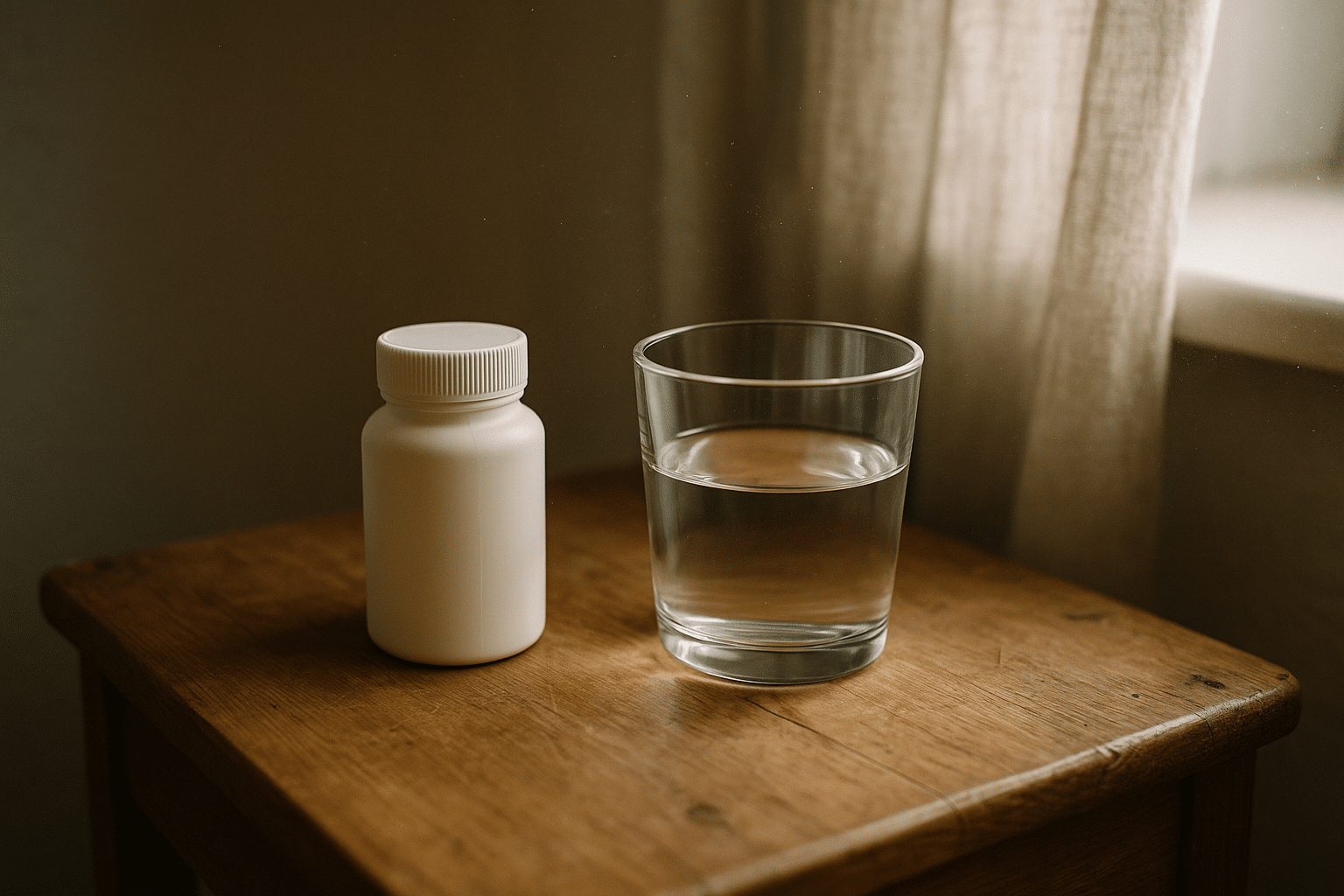
Pre-exposure prophylaxis, commonly called PrEP, is preventive medicine taken before potential exposure to HIV. Think of it as a seatbelt for your immune system: you hope you never need it, but having it in place dramatically lowers risk when life throws a hard brake. Modern PrEP combines evidence-based pharmacology with routine diagnostics to make prevention personal, adaptable, and practical. This article provides a clear path through three pillars—anatomy, pharmacology, and diagnostics—so you can understand how PrEP fits different bodies, schedules, and risk profiles without hype or confusion.
Here is the outline we will follow to navigate the topic and turn technical points into everyday decisions you can apply with your clinician:
– Anatomy: where and how HIV typically enters, what tissues are most vulnerable, and how local biology affects risk.
– Pharmacology: how PrEP agents work in the body, dosing approaches, drug levels at mucosal sites, side effects, and interactions.
– Diagnostics: the testing and monitoring that keep prevention safe, including HIV assays, kidney function checks, and STI screening.
– Practicalities: adherence tactics, travel and missed doses, switching regimens, and when to consider post-exposure measures or discontinuation.
PrEP is highly effective when taken as prescribed. Daily oral options reduce sexual transmission risk by about 99% in adherent users, while long-acting injectable formulations have shown very strong performance in randomized trials across multiple regions and populations. Effectiveness varies by adherence, drug levels in specific tissues, concurrent sexually transmitted infections, and partner viral load. Routine testing ensures PrEP is started and continued at the right times, and that any early HIV infection is not masked by partial medication exposure. By the end of this guide, you will have a grounded understanding of body barriers, drug behavior, and the lab roadmap that makes prevention both safe and sustainable.
Anatomy of Transmission and Protection
HIV transmission is a microscopic story that unfolds across distinct anatomical landscapes. The virus typically enters through mucosal surfaces—rectal, vaginal, cervical, oral—where a single layer (or few layers) of epithelial cells, immune sentinel cells, and microvessels form both a defensive wall and, under certain conditions, a doorway. The rectal mucosa, for example, is relatively thin and rich in immune cells, making receptive anal intercourse a higher per-exposure risk compared to many other routes. Cervicovaginal tissues, while thicker, can be affected by hormonal cycles, inflammation, and microabrasions that change susceptibility from week to week.
Local immunity and the condition of tissues matter. Microtrauma from friction, ulcerative lesions, or an untreated sexually transmitted infection can create microscopic breaches where HIV more easily encounters target cells such as CD4+ T cells and dendritic cells. Inflammation recruits more of these target cells into the area, which can amplify vulnerability even without visible symptoms. Circumstances such as condomless sex, presence of genital ulcer disease, or rectal inflammation can all increase risk, while consistent condom use, lubrication, and PrEP can reduce it substantially. Partner factors also count: higher plasma or genital viral load is associated with higher transmission risk, and effective treatment for a partner living with HIV dramatically cuts transmission likelihood.
In this context, PrEP acts within tissues where exposure occurs. Oral PrEP agents achieve concentrations in rectal and genital compartments sufficient to inhibit viral replication soon after exposure. Long-acting injectable PrEP maintains steady drug levels in blood and target tissues over weeks, creating a standing guard even when daily pill-taking would be challenging. The speed at which protective levels are achieved differs by tissue. With tenofovir-based oral PrEP, many guidelines note that steady-state protection for receptive anal sex may be reached within about seven days of daily dosing, while cervicovaginal tissues may require up to approximately 21 days. Event-driven dosing has strong support for individuals assigned male at birth engaging in anal sex, but it is not recommended for those with vaginal exposure risks due to pharmacokinetic differences in tissue penetration.
Risk is never uniform; it is anatomical, situational, and time-dependent. That is why the same person might benefit from different prevention strategies during different seasons of life—daily oral PrEP during frequent exposure periods, a long-acting injection during travel or high-activity months, or pauses with careful re-starting when circumstances change. Understanding the body’s entry points, the role of inflammation, and the dynamics of tissue drug levels turns an abstract idea—“prevent infection”—into a series of concrete, anatomical checkpoints where PrEP can make a measurable difference.
Pharmacology of PrEP: Mechanisms, Dosing, and Interactions
PrEP pharmacology hinges on putting the right drug, in the right amount, into the right tissues at the right time. Most oral PrEP relies on nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), such as tenofovir and emtricitabine. These analogs impersonate natural nucleotides used by HIV’s reverse transcriptase enzyme. When incorporated into viral DNA, they terminate the chain, halting replication before the virus can establish a foothold. Long-acting injectable PrEP uses an integrase inhibitor (e.g., cabotegravir) that prevents HIV from integrating its genetic material into host DNA, another critical step in establishing infection.
Distribution and persistence are crucial. Tenofovir-based oral PrEP tends to achieve higher concentrations in rectal tissue more quickly than in cervicovaginal tissue, which explains why daily dosing requires different lead-in times depending on exposure route. The half-life of active metabolites inside cells allows once-daily dosing for oral regimens. For the injectable integrase inhibitor, the extended-release formulation creates a depot that slowly releases medication, maintaining protective plasma and tissue levels for weeks between dosing visits. This regimen can be advantageous for those who struggle with daily pill-taking or anticipate periods of unpredictable exposure risk.
Dosing choices include daily oral dosing for all exposure types and event-driven “2-1-1” dosing for some individuals assigned male at birth who have infrequent anal sex exposures, with clinician guidance. Long-acting injectable dosing begins with an initiation phase (which may include an optional oral lead-in) followed by maintenance injections at scheduled intervals. People should work with clinicians to assess candidacy for each option, considering anatomy of exposure, frequency, and personal preferences. Effectiveness data show high protection rates when regimens are taken as prescribed; in some trials, the injectable option reduced HIV incidence relative to oral PrEP in certain populations, underscoring the value of multiple choices tailored to adherence patterns.
Safety profiles are generally favorable. Oral NRTI-based PrEP can cause mild, transient gastrointestinal symptoms in the first weeks for some users. Small, reversible decreases in kidney filtration markers and modest changes in bone mineral density have been observed with certain tenofovir formulations; baseline and periodic monitoring help catch concerns early. Long-acting injections commonly cause local reactions—soreness, nodules, or redness—that usually improve within a few days. Drug-drug interactions are limited but not zero: medications that affect renal transporters may influence tenofovir exposure, certain anticonvulsants or rifamycins can lower integrase inhibitor levels, and herbal supplements with enzyme-inducing effects may matter. Alcohol does not directly interfere with PrEP’s mechanism, but it can complicate adherence; practical strategies like pairing doses with daily routines can help.
In short, PrEP pharmacology is about aligning molecular tactics with life logistics. By understanding how these agents block replication at different stages, how fast they distribute into key tissues, and how long they last, individuals and clinicians can select a regimen that balances potency, convenience, and safety—without overpromising, and with clear-eyed attention to personal habits and health history.
Diagnostics and Monitoring in PrEP Care
Diagnostics are the backbone of safe PrEP. Before starting, a laboratory-confirmed negative HIV test is essential. Most programs use fourth-generation antigen/antibody assays at baseline to detect both established infection and many acute cases. If there is recent high-risk exposure or symptoms consistent with acute infection—fever, rash, sore throat—clinicians may add an HIV RNA test to minimize window-period uncertainty. Ongoing testing every three months (or per local guidance) reduces the chance of unrecognized seroconversion, which is important because taking partial PrEP during early HIV infection can complicate treatment and resistance management.
Kidney function testing (typically estimated glomerular filtration rate and serum creatinine) is standard for oral tenofovir-based PrEP. Baseline assessment ensures filtration capacity is appropriate for the selected formulation, and periodic checks—often every six months, or more frequently if there are risk factors—monitor for small changes that, while uncommon, deserve attention. Bone health may be discussed in individuals with osteoporosis risk; where relevant, clinicians might consider vitamin D status, calcium intake, or alternative regimens. For long-acting injections, while kidney monitoring is not typically central, baseline HIV testing and continued frequent screening are especially important because dosing intervals are longer and residual drug persists for months.
Hepatitis B and C considerations are integral. Screening for hepatitis B surface antigen and antibodies informs vaccination decisions and helps guide care because certain oral PrEP agents also have activity against hepatitis B. Stopping these agents abruptly in people with chronic hepatitis B can lead to flares; coordinated management avoids complications. Hepatitis C screening is recommended based on risk; people who inject drugs benefit from integrated prevention that includes sterile syringe access, opioid use disorder treatment where appropriate, and routine HCV testing.
Sexually transmitted infection screening complements HIV prevention, as STIs like gonorrhea, chlamydia, and syphilis can increase susceptibility through inflammation or breaks in mucosa. This typically includes testing at relevant anatomical sites—throat, rectum, urine or vaginal/cervical swabs—guided by sexual practices. Many programs recommend screening every three to six months. Pregnancy testing is appropriate for those who could become pregnant, paired with counseling on the safety of specific PrEP options during pregnancy and breastfeeding. Vaccinations—hepatitis A and B, human papillomavirus, and others per age and risk—round out the preventive package.
Practical diagnostics also consider access. Some settings offer clinic-based rapid tests with confirmatory laboratory follow-up; others support home sample collection or self-testing with telehealth. Whatever the pathway, documentation of results, reminders, and integration with pharmacy refills help avoid gaps. With a reliable testing cadence and clear communication, diagnostics transform PrEP from a static prescription into a dynamic, monitored prevention plan that evolves with a person’s life and risk patterns.
Adherence, Access, and Real-World Scenarios
Effectiveness in studies translates to real life when adherence fits daily rhythms. People use creative, simple anchors to keep doses consistent: linking the pill to brushing teeth, setting a phone reminder that vibrates discreetly, or using a travel-sized pill case clipped to keys. For injections, pairing clinic visits with existing routines—paydays, workout schedules, or community events—can reduce missed appointments. Missed oral doses happen; a practical rule many clinicians share is to take the dose as soon as remembered unless it is very close to the next scheduled time, and to avoid doubling up unless advised. For event-driven regimens used by some individuals assigned male at birth for anal sex, the structured “2-1-1” pattern requires planning around anticipated exposure; when life gets unpredictable, daily dosing or a switch to long-acting injections can simplify things.
Stopping and re-starting PrEP safely is part of the journey. If exposure risk decreases—say a monogamous relationship with a partner who is durably undetectable on HIV treatment—a person may pause with guidance on how long to continue after the last potential exposure. Re-start plans factor in lead-in times for tissue protection: daily oral regimens may need about seven days for rectal protection and about 21 days for cervicovaginal protection, while injectables follow clinic-set initiation schedules. After a high-risk exposure without adequate PrEP coverage, post-exposure prophylaxis (PEP) is time-sensitive and usually initiated within 72 hours; many programs maintain streamlined links between PEP and ongoing PrEP to support continuity.
Access and affordability vary by setting, but multiple public and private pathways can reduce out-of-pocket costs. Community clinics, telehealth services, and mail-order pharmacies help people in rural or busy urban environments maintain timely refills or injections. Confidentiality matters; discreet packaging, private lab portals, and respectful clinical environments encourage retention. Stigma remains a barrier for some; normalizing PrEP as routine preventive care—akin to contraception or vaccines—helps shift the narrative from judgment to agency. Evidence does not support the idea that PrEP universally increases risky behavior; while some individuals may change condom use, overall public health benefits include fewer HIV transmissions and more frequent STI screening that finds and treats infections earlier.
Finally, prevention is bigger than pills or injections. It includes open conversations with partners, periodic reassessment of goals, and attention to mental health and substance use that may affect adherence. Useful prompts for self-check-ins include:
– Did my exposure patterns change this month?
– Are reminders and refill systems still working?
– Do I have upcoming travel or schedule shifts that call for a different regimen?
– Have I noticed side effects that I should discuss at my next visit?
With a flexible plan, PrEP becomes not just a medication, but a sustainable practice that fits the contours of real life and respects each person’s autonomy.