Exploring the Role of Chronic Pain Support Clinics
Chronic pain shapes routines, decisions, and relationships—often in ways that outsiders cannot see. Support clinics exist to counter that invisibility with coordinated care that targets pain drivers, builds coping capacity, and restores participation in daily roles. Their approach is not a quick fix; rather, it is a structured path that blends medical decision-making with therapy and rehabilitation, aiming for meaningful improvements in function and quality of life.
Outline:
– The Landscape of Chronic Pain and the Clinic Model: why clinics exist and what to expect
– Pain Management in Practice: medications, procedures, and self-care
– Therapy in Clinics: mind-body approaches and behavior change
– Rehabilitation and Functional Restoration: movement as medicine
– Conclusion and Practical Next Steps: choosing and using a clinic
The Landscape of Chronic Pain and the Clinic Model
Chronic pain is common, complex, and costly. Population studies in multiple regions estimate that roughly one in five adults lives with persistent pain lasting longer than three months, with significant impacts on sleep, mobility, employment, and mental health. Costs include not only medical visits and medication, but also reduced productivity and lost opportunities. Support clinics emerged to address this complexity by bringing disciplines together—medicine, psychology, physical and occupational rehabilitation—under a single, coordinated plan.
Here is how the model typically works. Intake begins with a comprehensive history that explores pain onset, aggravating and relieving factors, prior treatments, and personal goals. Clinicians often screen for mood symptoms, sleep disturbances, and fear of movement, because these factors can amplify pain signals and shape behavior. Physical examination focuses on function—what you can do and what you avoid—alongside neurologic and musculoskeletal findings. Rather than treat pain as a single symptom, the clinic team maps a web of contributors: tissue sensitivity, deconditioning, stress, disrupted routines, and learned protective patterns.
A key feature is collaborative goal setting. Instead of aiming only for “no pain,” which may not be realistic for long-standing conditions, the team and patient select functional targets, such as walking for 20 minutes without a flare, cooking a simple meal, or returning to part-time work. Goals are tied to measurable outcomes and regular reviews. Many clinics use brief tools—like a 0–10 pain interference scale, a three-item pain intensity/engagement measure, or mobility tests—to track progress. This makes care adaptive, not static, and prevents long stretches of trial-and-error without feedback.
Expect the plan to be staged. Early steps might include pain education and gentle movement, then graded exposure to feared activities, and targeted medication or procedural trials when indicated. Coordination minimizes duplication and focuses on carryover into daily life. Benefits include:
– A single plan that aligns medical, therapy, and home strategies
– Timely course corrections based on outcomes rather than guesswork
– Emphasis on function, which patients often value as much as pain relief
In short, the clinic model aims to turn scattered efforts into an integrated program that respects biology, behavior, and context—three levers that, when pulled together, can move the needle.
Pain Management in Practice: Medications, Procedures, and Self-Care
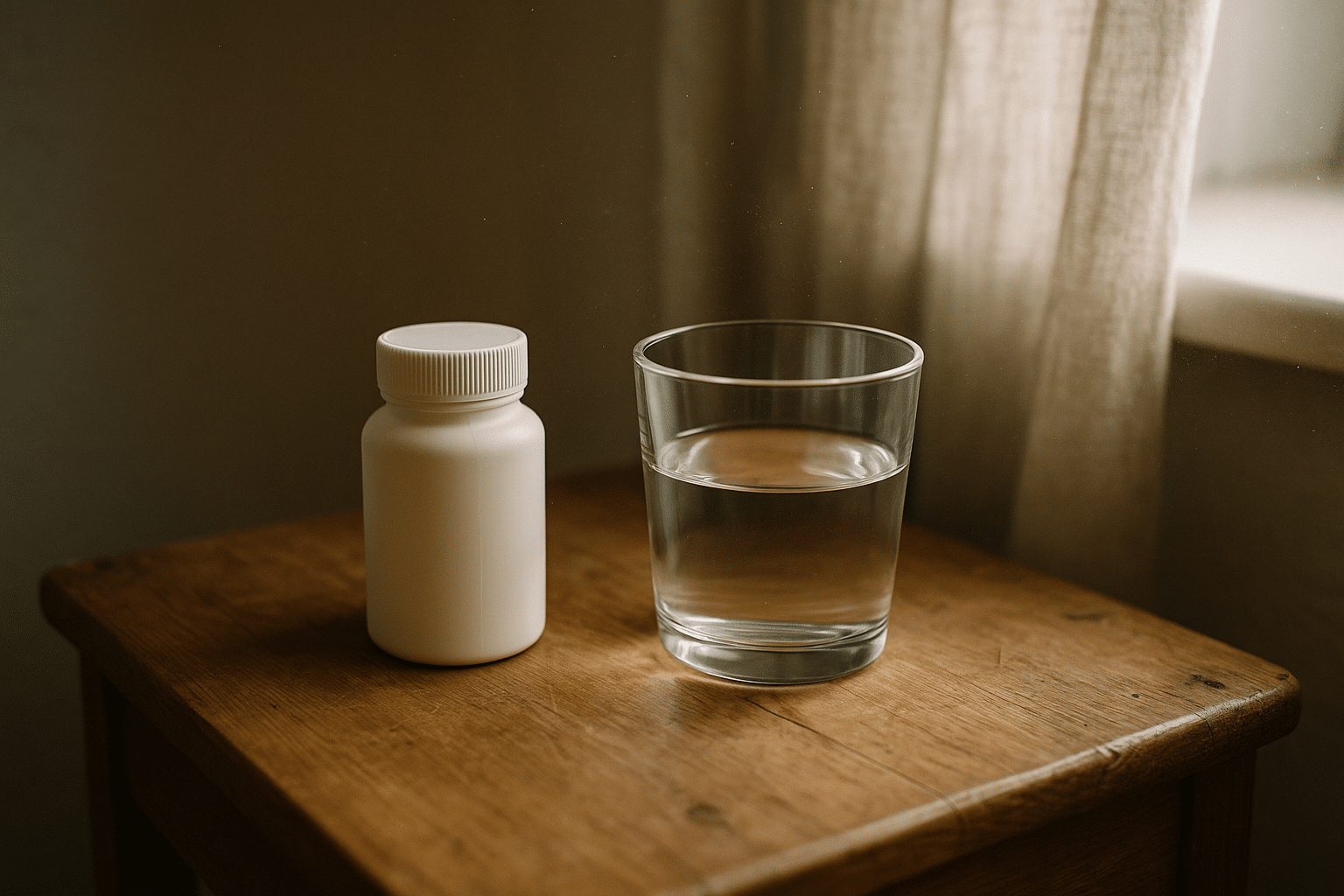
Pain management within support clinics balances symptom control with safety and long-term function. Medication strategies typically start conservative and proceed stepwise based on diagnosis, risk factors, and response. Common options include acetaminophen and nonsteroidal anti-inflammatory drugs for nociceptive pain, adjuvant agents such as certain antidepressants or anticonvulsants for neuropathic features, and topical preparations for localized symptoms. Evidence suggests that many medications produce modest average reductions in pain, and that even a 10–20 percent decrease can feel meaningful when combined with better sleep, movement, and coping skills.
More interventional steps—such as targeted injections—may be considered for specific conditions, especially when imaging and clinical signs align. Clinics tend to emphasize prudent selection, time-limited trials, and functional benchmarks rather than repeating procedures indefinitely. Opioid prescribing, where considered, typically follows careful risk-benefit discussion, screening for overdose risk, and a plan that includes monitoring, taper options, and non-drug supports. The guiding principle is stewardship: the right dose, for the right patient, for the right duration, if the expected benefits outweigh the risks.
Medication choices always live alongside self-management. Many patients report that consistent routines create steadier days than fluctuating doses. Useful non-drug measures include:
– Pacing and activity planning to avoid boom-and-bust cycles
– Sleep hygiene strategies that reduce nighttime awakenings
– Heat or cold for short-term relief during flares
– Gentle aerobic activity to increase circulation and mood
– Nutrition patterns that support energy and reduce irritability around meals
Comparing approaches helps clarify trade-offs. Medications may act quickly but can bring side effects; procedures can be targeted but often have time-limited effects; self-management builds resilience but requires practice. Clinics integrate these options by setting milestones: for example, trial an adjuvant medication for six to eight weeks while advancing a walking plan and practicing relaxation skills, then reassess pain interference, function, and side effects. If gains plateau, the team adjusts—perhaps emphasizing graded exposure and sleep strategies while tapering a medication that offers little additional value.
Data-informed care keeps expectations realistic. Few single treatments eliminate chronic pain, but layered strategies can improve comfort, confidence, and engagement. That layered approach—more orchestra than solo—defines how support clinics aim to deliver sustainable relief.
Therapy in Clinics: Mind-Body Approaches and Behavior Change
Therapy is a cornerstone of clinic-based care because pain is not only a sensory signal; it is an experience shaped by attention, beliefs, mood, and movement patterns. Numerous trials show that psychological therapies can reduce distress, enhance coping, and improve function. Cognitive behavioral therapy (CBT) helps patients notice and reframe unhelpful thoughts—like “any pain means damage”—and replace avoidance with planned, graded activity. Acceptance and commitment therapy (ACT) teaches skills for making room for discomfort while moving toward personal values, such as parenting, work, or creative pursuits, which can shrink pain’s footprint in daily life.
Mindfulness-based strategies target attention and arousal. By practicing nonjudgmental awareness of sensations and breath, patients often report less reactivity to spikes in pain. Pain neuroscience education, delivered in plain language, explains central sensitization, amplification, and the role of fear. When patients understand that increased sensitivity is not the same as ongoing injury, they are more willing to re-engage in movement—an essential step in rehabilitation.
Therapists frequently address fear-avoidance and catastrophizing, two patterns strongly associated with disability. Graded exposure turns feared tasks into manageable challenges. For example, someone who avoids bending might rehearse a small hip hinge with breath control, then progress to picking up a light object, then lifting a grocery bag. Each step is rehearsed between visits, tested in real environments, and logged to reinforce progress. Group formats can add peer support, normalizing setbacks and sharing practical tips.
Realistic outcomes matter. Meta-analyses generally find small-to-moderate improvements in pain intensity and function with CBT and related therapies, with stronger effects on mood and coping. Clinics build on this by embedding skill practice into the week: breathing drills before commutes, brief exposure sets during household tasks, and brief reflections before bed. Patients learn to spot early signs of a flare and pivot: reduce load, apply heat, hydrate, and use a pacing plan rather than stopping all activity.
Therapy is not about positive thinking or willpower. It is structured learning that changes how the nervous system prioritizes signals and how behavior influences tissue load. In this respect, psychology is biomechanics’ ally: one shapes attention and choices; the other shapes forces and capacities. Clinics knit them together so that what you learn in the chair transfers to what you do at the sink, stairs, and sidewalk.
Rehabilitation and Functional Restoration: Movement as Medicine
Rehabilitation translates intent into action. Physical and occupational therapists in support clinics assess mobility, strength, endurance, coordination, and the real-world tasks you want to perform. The plan typically blends flexibility work, graded aerobic activity, and strengthening targeted to the relevant kinetic chain. Early sessions may prioritize gentle range-of-motion and breath-coordinated movement to reduce guarding. As confidence grows, programs introduce load through isometric or eccentric exercises, then add complexity—balance, rotation, and task-specific drills.
Active care anchors the process because it creates durable change. Passive modalities—such as certain manual techniques or modalities delivering heat—may offer short-term relief, but the clinic’s goal is to convert that relief into training opportunities. For example, a brief manual treatment might reduce stiffness so that you can practice a squat pattern at low depth; that pattern then becomes a home exercise with two to three sets most days. Activity is dosed like medication: intensity, frequency, and progression are planned, recorded, and adjusted.
Occupational therapy bridges clinic gains with home and work. Practitioners evaluate task setup, body mechanics, and energy conservation. Small changes—like raising a work surface, using a neutral-grip tool, batching errands, or alternating standing and seated tasks—can reduce cumulative load. Adaptive strategies do not mean surrender; they create a runway for capacity building. As tolerance improves, supports can often be reduced or removed.
For those deconditioned by long avoidance, graded activity and exposure strategies slowly increase time-on-task. Aquatic therapy can be useful when weight-bearing is difficult; the buoyancy allows joints to move with less compression, and the water’s viscosity adds gentle resistance. When balance is a concern, practices include narrow-stance drills, single-leg stands near a counter, and step-downs with support. Flare planning is built in so that a setback does not derail the entire week:
– Adjust load by reducing volume or intensity, not stopping entirely
– Swap to low-impact options, like cycling or water walking
– Use brief recovery practices—breath work, heat, or a short walk—before resuming
Clinics measure function as carefully as pain. Timed sit-to-stand tests, walking speed, and patient-reported interference scores provide concrete feedback. Improvements here often precede large changes in pain intensity, yet they correlate with better participation and mood. By treating movement as medicine—with a dose, a schedule, and side-effect monitoring—rehabilitation turns possibility into habit.
Conclusion and Practical Next Steps: Choosing and Using a Clinic
Finding a clinic that fits your needs starts with clarity about goals and values. Are you aiming to walk a certain distance, return to a craft, sleep through the night, or reduce missed workdays? Write these down and bring them to the first visit. Look for programs that provide coordinated care with clear communication among clinicians, emphasize functional goals, and use outcome measures to guide adjustments. Ask how progress is tracked, how home practice is supported, and what happens if a plan is not working as expected.
Access and logistics matter. Consider location, appointment times, and whether telehealth complements in-person visits for education or check-ins. Insurance coverage and costs should be transparent; many clinics offer phased programs so that time-intensive components happen early, with spacing as you gain skills. If you are a caregiver, ask how you can support pacing, practice, and follow-through at home without overstepping autonomy. If you are an employer or educator, discuss reasonable accommodations that enable participation while recovery continues.
As you evaluate options, watch for signs of a good fit:
– Plans that integrate medical, therapy, and rehabilitation rather than isolate them
– Education that explains the “why” behind each step, not just the “what”
– A willingness to taper or discontinue treatments that do not add value
– Respectful discussion of risks, benefits, and uncertainties
Equally, be cautious if promises sound absolute, if procedures are repeated without clear goals, or if you are discouraged from asking questions. Sustainable gains usually come from layered strategies practiced consistently over weeks to months. A useful mindset is to treat the clinic as a training ground: learn skills, test them in your real environment, and refine them with feedback.
Summary for people living with pain and those who support them: coordinated clinics can help you move from scattered efforts to an integrated plan that respects your biology and your life. Expect thoughtful assessment, realistic targets, and steady skill-building. Measure the outcomes that matter to you. With a team that listens and a plan that evolves, comfort and capability can grow together.